Homepage \\ Meet Our Doctors
Meet Our
Doctors
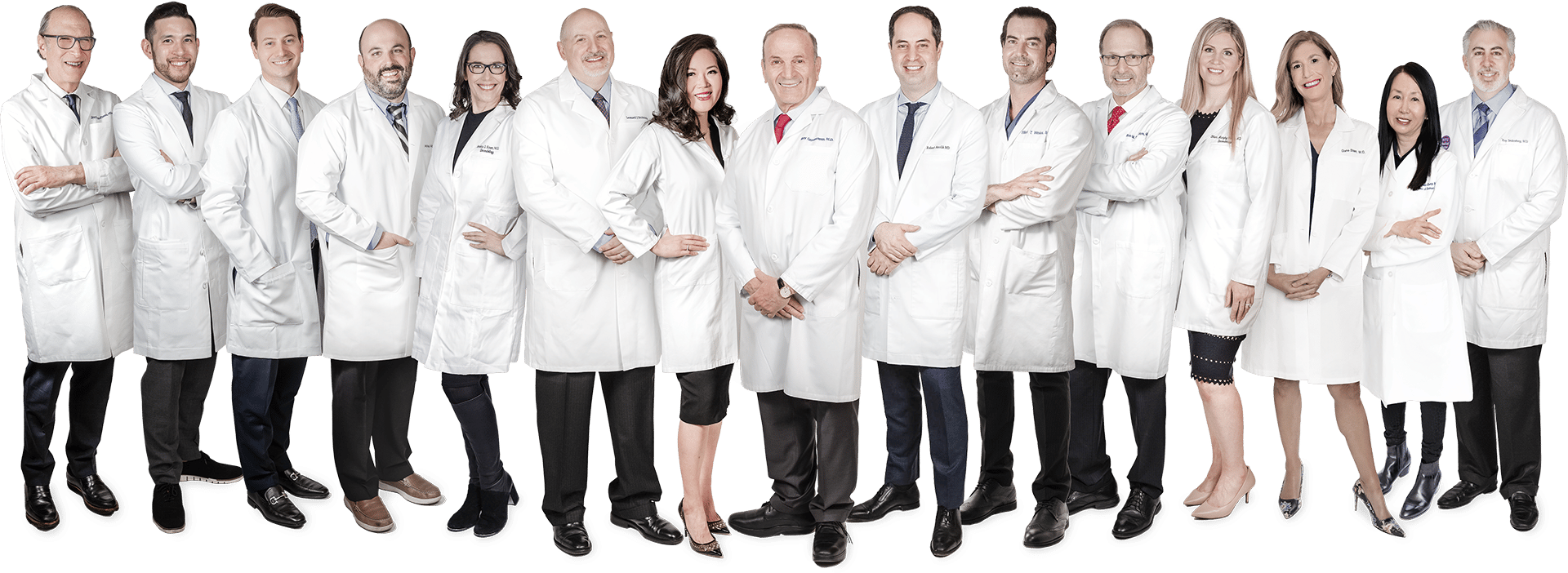
Our board-certified dermatologists are all fellowship trained and uniquely trained in lasers and technology, cosmetic and medical dermatology, and skin surgery. Together they are highly acclaimed world experts with thousands of articles published, countless TV and media appearances, and hundreds of years of combined experience.
Aesthetician
EWA SZTUKOWSKA
Aesthetician
patient approved
Trusted Worldwide
patient approved
Trusted Worldwide
Our 30,000+ sq foot dermatology center in New York is the most comprehensive, state-of-the-art laser and cosmetic skin surgery center in the world. Over the past 30 years we have contributed to the development and testing of many devices, fillers and treatments that are now standard care, so our patients know they are always receiving the most innovative, cutting-edge treatment available.
laser & skin surgery
center of new york
Contact us
Manhattan:
317 East 34th Street New York, NY 10016
Monday – Friday: 8:00am – 5:00pm
Saturday & Sunday: September through June by appointment only
Same-Day Appointments Now Available
Southampton:
325 Meeting House Lane, Bldg. 1, Ste. C Southampton, NY 11968
Monday - Wednesday, Friday: 9am - 4:30pm
Thursday: 9am - 5pm
Saturday October 1, 2022: By Appointment Only
Same-Day Appointments Now Available
Pay Online for Patients of Drs. Geronemus, Anolik, Bae & Seidenberg
Pay Online for Patients of Drs. Abraham, Bernstein, Krant, Shelton, Stern, Weiss, Hoffman, Shim, Murphy-Rose, Wilson, and Petratos
By LASER & SKIN SURGERY CENTER OF NEW YORK® | © 2024 All Rights Reserved. Design & Development by Goldman Marketing Group | Sitemap | Privacy Policy | The information available on this web site is provided for informational purposes only. This information is not intended to replace a medical consultation where a physician's judgment may advise you about specific disorders, conditions and or treatment options. We hope the information will be useful for you to become more educated about your health care decisions. If you are vision-impaired or have some other impairment covered by the Americans with Disabilities Act or a similar law, and you wish to discuss potential accommodations related to using this website, please contact us at (212) 941-5055.
*MDs perform 100% of all medical and cosmetic treatments.